RSV IS A LEADING CAUSE OF HOSPITALIZATION IN INFANTS UNDER 2 YEARS IN CANADA2†
A severe RSV infection has the potential to hospitalize ANY infant in their first season3–5
RSV is the main cause of LRTIs in young children worldwide and may cause severe respiratory infections, mainly as bronchiolitis and pneumonia.
Most cases of bronchiolitis are caused by RSV.
A severe RSV infection may lead to hospitalization, serious complications (such as respiratory failure), and other sequelae, such as wheezing, asthma, and hyperreactive airways.6,7
It’s time to raise awareness of RSV and its threat to ALL infants.
RSV EXPERT SERIES
Watch leading physicians discuss the latest information on RSV
A SEVERE RSV INFECTION CAN STRIKE ANY CHILD3–5
Any infant can be hospitalized in their first season3–5
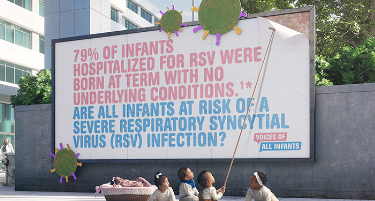
79%
RSV can affect infants who are born at term and are healthy
79% of infants hospitalized for RSV were born at term with no underlying conditions.1*
14x
RSV is a leading cause of hospitalizations in infants
In one Canadian study, infants under 2 years were 14 times more likely to be hospitalized due to RSV than influenza.2†
1 in 4
RSV symptoms can be life-threatening
Healthy infants with no underlying conditions have been admitted to the ICU due to RSV, as seen in a US study, which found that 1 in 4 of such infants required intensive care.8‡
95.5%
RSV places a burden on the healthcare system in Canada
In a study of RSV hospitalizations in Alberta, 95.5% of infants received supplemental oxygen and 13.4% were admitted to the ICU. The average length of stay in the hospital was 5.7 days overall, and 6.5 days for patients who went to the ICU.9§
RSV FREQUENTLY ASKED QUESTIONS

While it is true that the majority of infant cases of RSV result in mild illness, that can be managed at home or by symptomatic care10, RSV is a leading cause of respiratory hospitalization in infants under 2 years of age in Canada.2†
A severe RSV infection may develop into bronchiolitis and pneumonia,6 and as many as 1–2% of children younger than 6 months of age with RSV infection may need to be hospitalized.10 Given the potential for a severe RSV infection to affect ANY infant in their first season,3–5 we should remain vigilant for the health of all infants.
RSV is one of the most common causes of childhood illness.10 In one Canadian study, infants under 2 years were 14 times more likely to be hospitalized due to RSV than influenza.2†
Infants with congenital heart disease, chronic lung disease, suppressed immune systems, neuromuscular disorders and prematurity are at greater risk of developing a severe RSV infection.10 However, all infants are potentially at risk of developing a severe RSV infection.3–5 In fact, in one study, the majority (79%) of infants who were hospitalized from RSV were born at term and otherwise healthy.1*
Almost all children will experience their first RSV infection by two years of age, so it is something parents should be informed about.11 Patients should be aware of how RSV is transmitted, be able to spot signs of a severe infection, and know when to seek medical assistance.
Since a severe RSV infection can potentially affect any infant,3 remind parents of the simple ways they can help prevent RSV hospitalizations, such as limiting contact with siblings and other children with respiratory tract infections.11
Armed with knowledge, parents can take steps related to hygiene to help reduce the risk of their infant contracting RSV, and will know to act quickly if they suspect their child is becoming seriously ill.
RSV is mostly spread by children, due to a combination of factors. Children have higher infectious viral loads than adults, with longer durations of infection. Additionally, children are more likely to spend time with individuals in their own age group, who are more susceptible to infection with RSV.12 Research shows that infants with older siblings are more likely to become infected with RSV than firstborns13 and that young children may continue to spread the virus for up to 4 weeks after their own symptoms have resolved.14
RSV can spread when an infected person coughs or sneezes and infected respiratory droplets enter the body of another person through their eyes, nose, or mouth. The virus can also be transmitted by touching a contaminated surface, like a doorknob, and then touching the face before washing the hands.14
HOW CAN WE HELP LIMIT THE SPREAD OF RSV, STARTING TODAY?
While we can’t predict which healthy infants will be affected by a severe RSV infection,3–5 we can take steps to help limit infants from coming into contact with the virus in the first place.11
Read on for recommended hygiene measures to help understand and prevent RSV transmission.
An infant’s first RSV season (typically November to March) poses a potential threat to their health11,15
RSV often spreads to infants via contact with infected older siblings or other children12
Infants can catch RSV from contaminated surfaces and close contact with infected people12,14
Help parents to recognize early symptoms of RSV and know when to seek urgent medical attention16
Try to avoid close contact between the infant and siblings, friends and relatives with cold symptoms11
Cover coughs and sneezes with a tissue or upper arm sleeve – not with hands17
Wash hands often with soap for 20 seconds to prevent transmission11
Regularly clean and disinfect surfaces that infants touch or share with siblings17
ED=emergency department; ICU=intensive care unit; LRTI=lower respiratory tract infection; RSV=respiratory syncytial virus.
* Data from a 5-year, prospective, population-based surveillance of children hospitalized with RSV between October 2000 and March 2005. Among 559 RSV-hospitalized infants aged <24 months, 79% were previously healthy.
† Data extracted from the Canadian Discharge Abstract Database from 2003 to 2014 using a regression model to estimate respiratory hospitalizations attributable to influenza, RSV and other respiratory viruses.
‡ An observational retrospective cohort study of preterm and term infants <6 months of age that assessed the costs of RSV hospitalizations, severity, and costs for the 2011 to 2014 and 2014 to 2017 RSV seasons.
§ A prospective, observational, survey-based analysis of the burden of RSV. Infants included in the study were <1 year of age and were hospitalized with a confirmed diagnosis of RSV/LRTI (N=67).
References: 1. Hall CB, et al. Pediatrics 2013;132(2);e34a–38. 2. Schanzer DL, et al. Influenza Other Respir Viruses 2018;12:113–21; doi: 10.1111/irv.12497. 3. Arriola CS, et al. J Pediatric Infect Dis Soc 2020;9(5):587–95. 4. Pisesky A, et al. Incidence of Hospitalization for Respiratory Syncytial Virus Infection amongst Children in Ontario, Canada: A Population-Based Study Using Validated Health Administrative Data. 2016 Mar 9;11(3):e0150416. doi: 10.1371/journal.pone.0150416. 5. Buchan SA, et al. Pediatr Infect Dis J 2019 Apr;38(4):362–69. 6. Bianchini S, et al. Microorganisms 2020;8:2048; doi:10.3390/microorganisms8122048. 7. Canadian Paediatric Society. Available at: https://cps.ca/en/documents/position/bronchiolitis. Accessed August 23, 2022. 8. Krilov LR, et al. Am J Perinatol 2020;37(2):174–83. 9. Mitchell I, et al. Can Respir J 2017; Article ID 4521302, https://doi.org/10.1155/2017/4521302. 10. Centers for Disease Control. Available at: https://www.cdc.gov/rsv/clinical/index.html. Accessed June 8, 2022. 11. Robinson JL, et al. Canadian Paediatric Society. Paediatr Child Health 2015;20(6):321–26. 12. Yamin D, et al. PNAS 2016;113:13239–44. 13. Jacoby P, et al. Epidemiol Infect 2017;145:266–71. 14. National Collaborating Centre for Infectious Diseases. Available at: https://nccid.ca/debrief/respiratory-syncytial-virus-rsv/. Accessed June 8, 2022. 15. Reeves RM, et al. J Infect 2019;78(6):468–75. 16. Centers for Disease Control. Available at: https://www.cdc.gov/rsv/about/symptoms.html. Accessed June 8, 2022. 17. Centers for Disease Control. Available at: https://www.cdc.gov/rsv/about/prevention.html. Accessed June 8, 2022.